Featured Patient Story
Stroke victim’s life is saved by rapid and experienced response at Washington Hospital
“Everyone certainly gave me the best possible care,” said grateful patient
Video at
https://youtu.be/IHF4fk9NGF0
Feel fine Monday. Stroke and surgery Tuesday. Up and walking Wednesday. Home Friday. Back to work Monday. Whew. Is that possible? “Yes, and it’s what happened to me,” said Julie Nghiem of Fremont, a stroke victim who will always be grateful to the best care possible––all thanks to Washington Hospital. The scary story began one morning last August when this healthy and active mom of two boys, who works at Mission Hills Middle School in Union City, “became dizzy like never before, my left eye became shut and then I was feeling paralyzed.” Next thing you know, thanks to prodding from co-workers, Julie was in an ambulance and headed for the Washington Hospital Emergency Department. Click through our photos and find out more about the rapid, experienced and coordinated response that saved Julie’s life.

At 8:55 a.m., 911 was called, and she arrived at the Washington Hospital ED at 9:24 a.m. “The Emergency Medical Services team bringing Julie communicated that a stroke was suspected, so we issued a Code Neuro internally,” said Lin Naing, MD, a specialist in emergency medicine at Washington Hospital. “Decisions in cases like this must be made very fast, so our team was ready at the ambulance bay.” That team included a pharmacist, lab technician, stroke nurse, emergency nurse and more. “Experience counts,” added Naing, “and we certainly know the drill. We had to get her to the right imaging, the right staff and the right doctors immediately. Every second, thousands of her brain neurons were dying from lack of blood supply.”

“We have a great alert system, so we were ready when Julie arrived,” recalled stroke nurse Carla Graves, RN. “Our stroke nurses assess anyone coming into the ED who’s suspected of stroke, and we also provide a daily assessment of inpatients that have signs and symptoms of strokes. Washington Hospital really stands out by having a team of nurses 24/7 exclusively dedicated and specifically trained for this care.”

Ian Kelly, radiologic technologist, is pictured with one of the Hospital’s CT (computerized tomography) scanners. “Our department’s role was to manage the CT imaging of the patient’s brain, and to get this imaging accomplished as quickly as possible and in close collaboration with the care team.”

Washington Hospital neurologist Charan Singh, MD, was on call that day. “I had just completed morning rounds and was with a patient in my office across the street,” Singh recalled. “The code went out, and I immediately rushed over to the CT scanner. From this imaging, we determined Julie was having an ischemic stroke, which is an obstruction of blood flow to the brain, or blood clot.” Singh made the call to administer a drug therapy called tPA (tissue plasminogen activator), which helps dissolve blood clots. “Julie was getting more lethargic, and we wanted to start tPA right away,” said Singh, who noted the team’s experience in responding to strokes. “Our stroke program has been around for many years and we are very proud of our timeliness for interventions and treatments. And, our complication rates are very, very low.”

Pictured is Peter Liang, PharmD, clinical pharmacist, part of the stroke team alerted when the Code Neuro was originally called. A clinical pharmacist, along with physicians and nurses, helps assess a patient’s eligibility for the tPA therapy, which includes reviewing the patient’s medication history for drug interactions and any bleeding risks, depending on type of stroke. After team assessment, Peter facilitated the timely preparation and delivery of the medication to the patient for administration––time is of the essence in the treatment of a stroke.
Incredibly, from Julie’s ED arrival to CT scan to receiving the drug, only 24 minutes had elapsed!
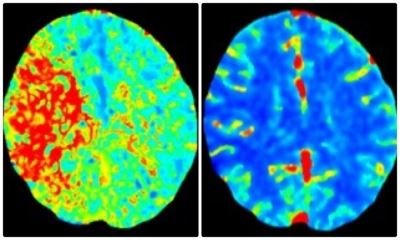
Next up in the fast-moving chain of events was more advanced brain imaging to determine if surgery was required: a CT angiogram and CT perfusion. This color-coded perfusion scan showed the area of Julie’s brain that was inadequately supplied (or perfused) with blood—the red area pictured left. A different but essential view showed that same large area of brain tissue has normal blue color (right). This meant that the red, injured area of her brain could be saved from permanent damage if its blocked blood flow could be emergently restored.

Neurosurgeon Jeffrey Thomas, MD: “Within two hours of Julie arriving at the ED at 9:24 a.m., she was in surgery and on the cath lab table,” he recalled. “Since imaging showed that two large arteries in her brain were blocked, surgery was absolutely required. The location was crucial, and she was going downhill. The initial symptoms were becoming more serious, signaling a larger stroke that was now likely to result in death.”
Instead of open brain surgery, this was a less-invasive interventional neuroradiology surgery in which Thomas planned to remove what was a very large blood clot clogging the brain arteries, and open the passages that were occluded or narrowed. It was a sophisticated and dangerous procedure that required extraordinary skill and experience by everyone on the team, from anesthesia to cath lab. “First, we made a keyhole incision in her groin, and then threaded flexible catheters through arteries in her body, navigating through her neck and into the brain,” Thomas said. “Then, we pulled out the clot blocking her middle brain artery and used a tiny balloon to open the blocked arteries. In combination with the tPA medicine, this is the most effective action to take, but it must be done quickly.”
The brain clot was extracted at 12:02 p.m.––less than three hours after Julie’s arrival in the ED. “Rapid diagnosis and rapid treatment are essential to keep stroke patients from going downhill or dying,” added Thomas, medical director of cerebrovascular and neurointerventional neurosurgery.
The surgery was a great success. “I was with Julie in the ICU waiting for her when she came out of the operation,” said stroke nurse Graves, “and I saw that her left arm and left leg were starting to move, even while sedated. To see this gave us tremendous hope and some assurance that she would be OK.”

“It really was confusing and unclear why such a young and healthy person would have a severe stroke,” said Jack Rose, MD, neurologist at Washington Hospital and Washington Health Medical Group. Julie sees Rose regularly for follow-up care. “We had to discuss her family history, as others in her family have had strokes,” Rose explained. “What we determined was that she has a very uncommon condition called FMD, or fibromuscular dysplasia” –– a disease that causes one or more arteries in the body to have abnormal cell development in the artery wall. “She never had any symptoms prior to the stroke,” Rose added. “Moving forward, our goal is to provide her with the right treatments and preventive medicines to prevent future strokes.”

Julie is forever thankful to her co-workers for helping her seek medical attention right away. Here, she is pictured in the Mission Hills Middle School administration office with Melanie Kirksey, left, and Lata Nigam, right. She’s long-since been back to her busy life of kids, family and work. She checks her blood pressure twice a day and takes anticoagulant medications to prevent blood clots and another stroke. “Looking back, the whole experience seems sort of vague. I don’t remember a lot about what happened, but I do know that everyone certainly gave me the best possible care,” she said. “My colleagues, emergency medical services and everyone at Washington Hospital played an amazing role in quickly saving my life, and I am eternally grateful.”


